The New Paradigm in Mental Health – Scientific Review.
“Symptoms are, solely, an indicator of where the healing needs to begin.
Not, merely, a clinical indicator of pathology.”
The Downfall of The Old Paradigm.
In 2013, a letter was written by the Director of The National Institute of Mental Health (NIMH) stating that the NIMH would no longer fund the American Psychiatric Association (APA). This was just weeks before the APA was to release what has been called “the bible” of mental health, entitled Diagnostic & Statistical Manual of Mental Disorders; 5th ed. (DSM-5).
To some, this manual is the gold-standard in mental health, diagnostic criteria.
To the NIMH, and many of us in the field, the DSM-5 is flawed within the APA’s dismissal of contemporary, scientific evidence that it was provided.
That recognizes new discoveries within the mental health research.
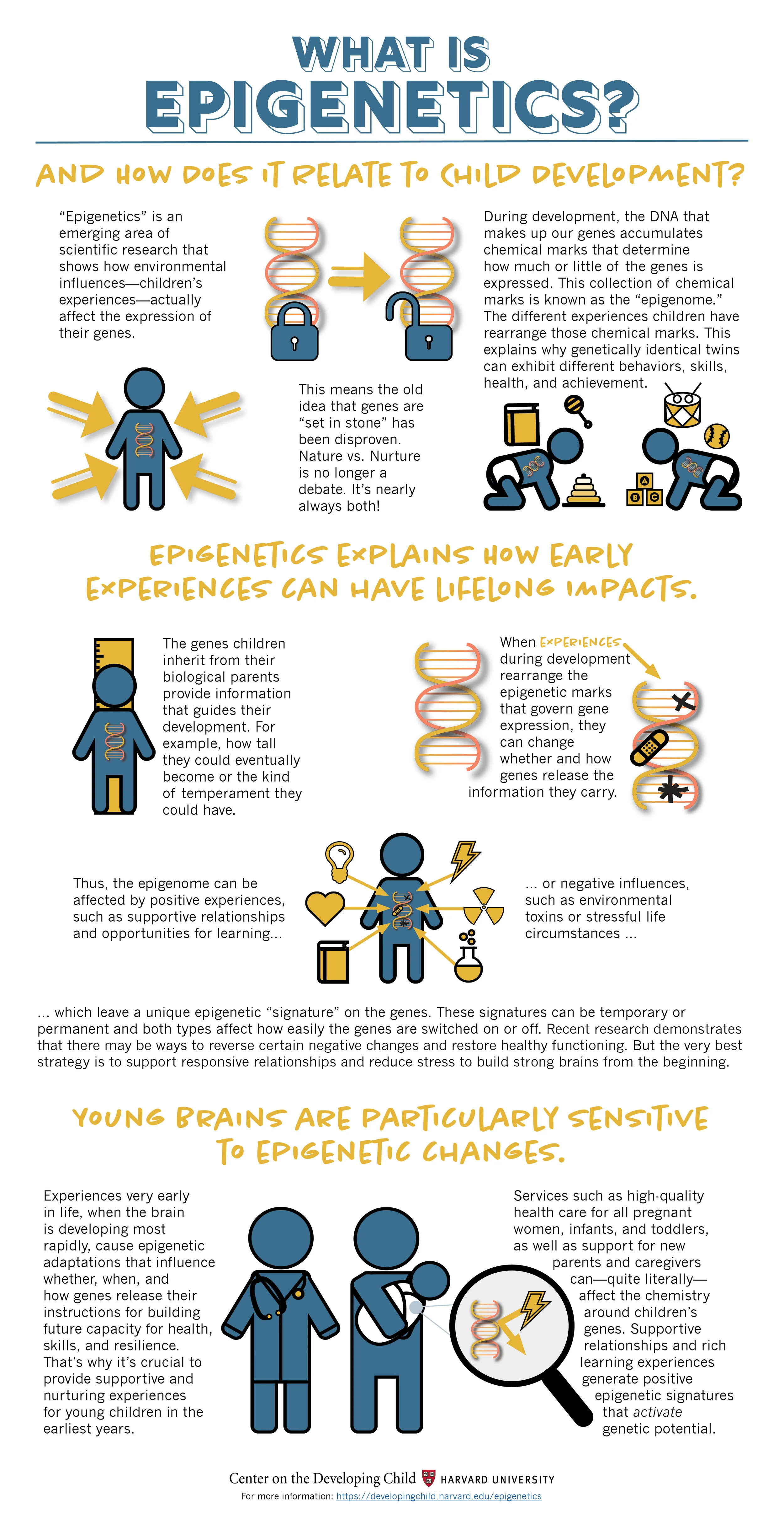
In the statement, the NIMH called out the APA for not including the new neurobiological research that clearly highlights environmental factors alter gene expressions during developmental years of childhood.
Which in turn, increases a person’s risk for mental health symptoms over genetic predisposition alone.
“The DSM diagnoses are based on a consensus about clusters of clinical symptoms, not any objective laboratory measure. In the rest of medicine, this would be equivalent to creating diagnostic systems based on the nature of chest pain or the quality of fever.”
“The weakness is its lack of validity.”
Thomas Insel, M.D. (Director of NIMH)
Then there is the American Counseling Association, and its petition with over 15,000 mental health professional signatures, who are critical of the DSM-5 due to its antiquated research.
That many of us providers consider not only focuses on dogmatic pathology, within the confines of medical management, but it also impedes clinicians from forward-thinking treatment models and progressive interventions.
In 2011, another letter was written to the APA, by the Chairman of the American Psychology Association, David Elkin.
Elkin stated that the APA’s approaches with the upcoming DSM-5 displays “little empirical support and/or research literature that is relatively recent.”
Which in turned garnered the support of over 50 mental health organizations to follow in protest of the APA and their DSM-5.
In short, opponents of the DSM-5 emphasize the APA’s dependency on the old paradigm.
It is even more heavily criticized for disastrously failing to include the mountain of neurophysiological science which sheds light on the significance of Adverse Childhood Experiences Studies and the direct, negative effects on psychopathology, neurobiology and persistent pathophysiology into adulthood.
The APA was further cited for neglecting to include, and utilize, newly developed research models.
Which have been devised to specifically investigate mental health issues in reliable and valid ways.
the New Paradigm; Part I: epigenetics versus Genetics.
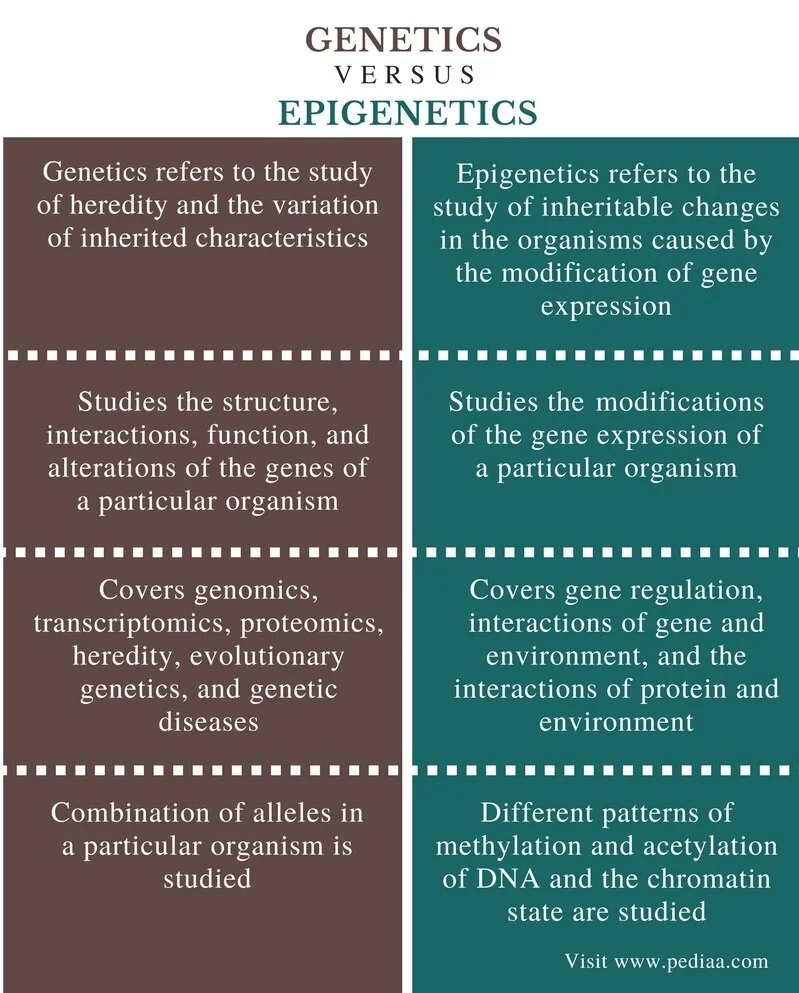
Previous genetic research, The Human Genome Project, set out to successfully classify and labeled genes.
It did not analyze for potential factors which influence DNA expression within genes.
Nor did it explore if gene behavior is fixed or flexible.
Suggesting a static way of rationalizing that mental health symptoms are largely genetic in nature.
However, mental health-epigenetic research, is demonstrating that this is far from accurate.
In that, environmental variables do indeed control gene expression and are very much connected to symptomatology than previously understood.
the New Paradigm; Part II; Psychology Meets Progressive Science.
Progressive research has recently uncovered that gene expression is indeed influenced by environmental factors.
These innovations, of the past two decades, are laying new groundwork within the field of psychology.
Stressing that the longstanding, “widely accepted, linear conception of the genome function” does not address the new breakthroughs verifying that “environmental and psychological factors regulate activity of our genome,” influencing psychopathology.
Implicating that a person’s risk for mental health symptoms is greatly influenced by factors outside their genetic susceptibility.
Underscoring that early life experiences and early-life stress, actually, has a significant and scientific effect in predicting mental health risk.
This new science, known as epigenetics, is revealing that environmental and psychological factors produce genetic mutations, called single nucleotide polymorphisms (SNPs), which methylate DNA.
Resulting in an increased risk-expression of mental health symptoms, after birth.
Epigenetic research brings the missing validity piece that the NIMH, and others, point out as the downfall of the American Psychiatric Association and it’s DSM-5.
In that, environmental/developmental factors have stronger predicting values related to mental health presentation over genetic inheritance.
Which is also generating new fields of research related into groundbreaking treatments that target the area of the altered polymorphisms. That are created by neurobiological imbalances linked back to adverse childhood experiences and chronic stress.
This process is now recognized as intergenerational trauma transfer and is the cornerstone of the importance in appreciating developmental trauma and adverse childhood experiences.
There is also the criticism that the APA’s DSM-5 lacks validity. Simply by not including the more rigorous, scientific investigation found in the current RDoC methodology (Research Domain Criteria).
Which has become the gold-standard in mental health research.
The significance of RDoC is within its framework that identifies five major valences which measure a variety of sub-constructs. Leading to a total of 39 primary variables which, concomitantly, contribute to mental health expressions.
RDoC methodology moves away from the current disease model of symptom-based diagnoses and more toward a biological-based findings that include modern research in the fields of epigenetics, neuroscience and behavioral sciences.
Epigenetics and The Importance of Developmental Trauma.
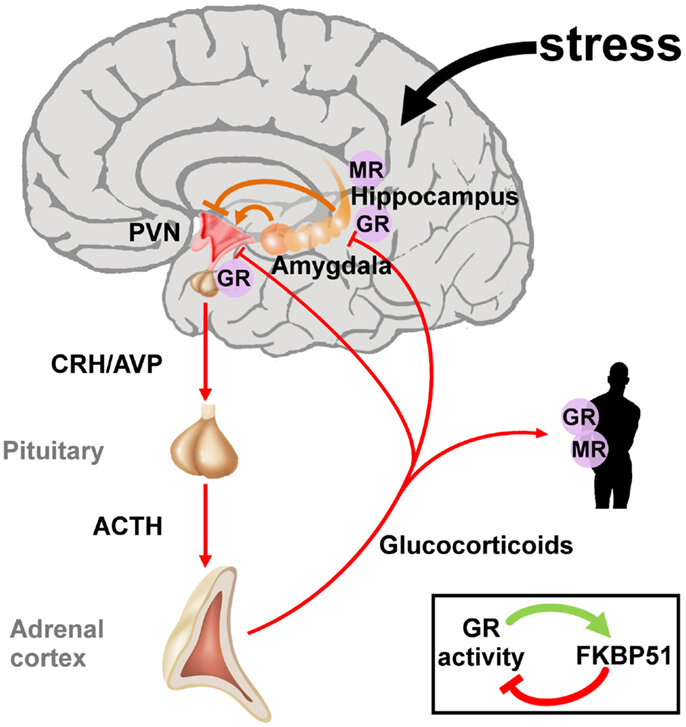
21st Century, RDoC, epigenetic research is clearly confirming that children who are exposed to adverse childhood events, and early life stress, have greater risk factors for developing “sympathetic adrenal medullary excitation followed by an increased hypothalamic pituitary-adrenal-cortical axis activity.”
Creating neurological imbalances that are carried into adulthood.
That chronically and negative effect neural pathways and generate the methylated polymorphism - SNPs - described above.
Resulting for altered gene expression, after birth and in early life stages.
Subsequently impacting the expression of mental health symptoms and inhibiting the management of negative arousal in adults.
Even years after the childhood trauma experience.
The NIMH went on to explain that the DSM-5 did not include over thirty years’ worth of evidence within Kaiser Permanente’s Adverse Childhood Experiences Studies (ACEs).
Which substantiate, without a doubt, that environmental risk factors matter more than genetic risk factors alone.
Now known as The Childhood Trauma Taskforce, formed in 2018, are the leaders of the past three, plus, decades who have provided the evidence that supports the RDoC methodology, and epigenetic research.
Fortifying the necessity of recognizing a new diagnostic criterias and approaches.
Back in 2009, this team formally proposed to the APA the Developmental Trauma Disorder, which recognizes the effects childhood maltreatment.
Only to have the APA reject the research and criteria for the upcoming DSM-5.
Which has brought commentary from experts in the fields of attachment, systems, and developmental psychology.
Going so far as calling the dismissal of Developmental Trauma Disorder as a “failure” in the proper identification and treatment of those suffering symptomatology.
The protest continues today even in the European mental health communities.
A Closer Look – Trauma, Epigenetics & Psychopathology.
Underscoring the impact of developmental trauma and epigenetics, there seems to be no more poignant statement than this quote published February, 2021:
“Over the past decade a rapidly growing body of literature has underscored the significant role of epigenetics in the sequelae of childhood maltreatment.”
Brown University, Department of Psychiatry.
Published twelve years ago was research that began to establish that early developmental maltreatment has a direct, causal connection between adverse childhood events and overall disease risk.
Which began to put forward that developmental trauma is associated with countless diagnoses, and epigenetic mutations play a key role over genetic predisposition.
For sake of conciseness, bipolar disorder will be the focus of further discussion related to the link between adverse childhood events, epigenetic triggers and risk for psychopathology.
Bipolar disorder, epigenetically, is associated with biomarkers that indicate a predisposition for shorter serotonin alleles [receptors] connected to methylation and histone mutation.
This 2020 article investigating Bipolar Disorder, examined those with such genetic biomarkers within two, stratified groups:
1) low Adverse Childhood Experiences Score (ACEs), and positive biomarker.
2) high ACE’s score, and positive biomarker.
The first cohort presented with far less bipolar symptomatology, lower rates of medical intervention and overall lower incidence of diagnoses.
In contrast, those subjects who presented with the same genetic predisposition for short alleles and higher ACE’s scores, had markedly higher symptomatology, higher rates of medical interventions and higher incidences of diagnoses.
Looking further into hereditary risk factors for bipolar disorder, investigators studied the offspring of parents who were diagnosed, and treated for, bipolar disorder.
Researchers specifically isolated those children with the genome identification associated with the disorder.
The researchers at The Department of Psychiatry and Behavioral Science, University of Texas, utilized RDoC methods to allow for outlying measures.
Which “emphasized the potential role of stress” on “DNA methylation (DNAm)” in the “functional relevance for the risk and expression of BD [bipolar] in youth.”
The Institute of Psychiatric Phenomics and Genomics, in Germany, explored stressful life events and the specific phenotype changes in those with bipolar disease.
At the time of publication, this was the first investigation examining “epigenome-wide methylation across time in bipolar patients and in relation to recent, non-traumatic stressful life event;”International Journal of Bipolar Disorders (2020).
Which explained, stressors catalyze phenotype changes that “have been associated with a worse course of BD [bipolar].”
Further advocating the the importance of continued efforts in understanding phenotype polymorphisms within the ramifications of neurobiological stress.
In another 2020 publication, investigators stated that there has been some progress in identifying hereditary factors with bipolar.
However, they also identified significant confusion within the “missing heritability” found in “genome-wide association studies.”
Childhood Trauma & Psychopathology Risk.
In 2003, ten years before the DSM-5 was published, the APA was made aware of the sizeable amount of literature “showing associations between childhood trauma and BD [bipolar] susceptibility and/or severity”.
Since then, further analysis indicates that those with bipolar polymorphism, in addition to higher incidence of adverse childhood experiences, are more vulnerable to increased symptomatology associated with bipolar.
Five years before the publication of the 2013 Diagnostic & Statistical Manual of Mental Disorders; 5th ed. (DSM-5), was this 2008 article; published in Bipolar Disorders: An International Journal of Psychiatry and Neuroscience entitled Beyond Genetics: Childhood Affective Trauma in Bipolar Disorder.
Concluding that “few susceptible genes have been associated with bipolar” and the genome research has produced “conflicting results”.
However, it clearly supports the escalating evidence that neurobiological consequences of childhood trauma lead to risk-presentation within the bipolar criteria over genetics alone.
Although bipolar was highlighted, the scientific literature broadly announces that:
“Even healthy adults who were victims in childhood remain at elevated risk for psychological problems.”
Research further states that developmental trauma and adverse childhood experiences induce “unstable changes in gene expression, neural circuit function, and ultimately behavior, and the maladaptation appear distinct between developmental versus adult exposure.”
In short, DNA methylation found in the epigenetic science, underscores the fact that “early adversities can engender long-term vulnerability for mental health problems” while altering gene expression.
New paradigm – Its Slowed adoption – The Consequences.
The past twenty years has provided an avalanche of evidence suggesting that developmental trauma, in the way of adverse childhood events, childhood victimization and childhood abuse or neglect, matters in the predictive values for psychopathology.
As compared to genetic predisposition - as once thought.
Unfortunately, this scientific information surrounding epigenetics, and its relationship to developmental trauma, is largely limited to research journals published within the past ten to twelve years.
Which most clinicians tend not to be actively exposed to.
In fact, studies suggest that it takes an average of seventeen years for novel information to make it to an average clinician.
Longer if you include incorporating current scientific findings into academic curriculums, continuing mental health education and training, even clinical practice supervision.
Which is slowed even more by mental health organizations who fail to include valid and reliable understandings of the new paradigms discovered in the mental health field.
Suggesting that current treatment conceptualization is likely outdated.
The significance of this fact is keenly pointed out by Dr. Edward Baker, from the Kings College of Department of Psychology, Institute of Psychiatry and Psychology of Neuroscience.
Who proclaims the importance of the new paradigm of epigenetics and trauma, over the old genetic, symptomatology paradigm.
In that, “promising” evidence is suggesting that “adversity related DNAm [polymorphisms],” that is linked to mental health epigenetics may be a “reversible mediator”.
Permitting for discoveries in approaches that allow for the remission of symptoms.
Not just symptom management.
Further establishing that current treatment models and therapeutic approaches must be reexamined.
Peripheral Inflammation – A New Paradigm in Treatment; Part I.
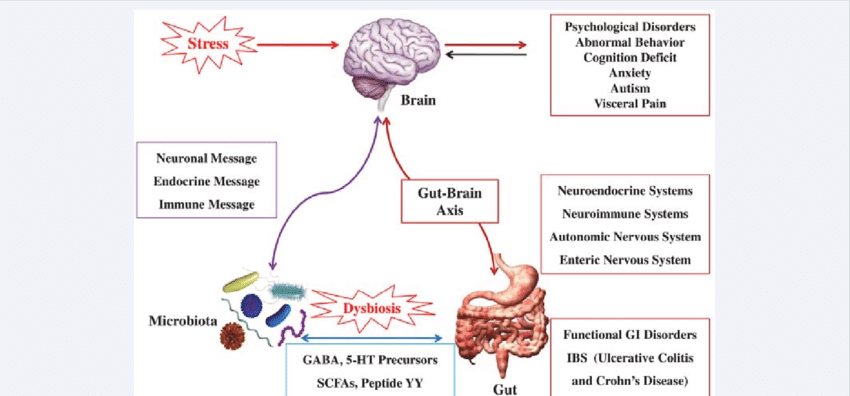
Let’s look more closely at how peripheral and enteric nervous system inflammation, created by methylation and polymorphism, is associated with bipolar symptoms.
Virome research, or gut microbiome studies, suggest that those who suffer bipolar disorder have microbiome imbalances within the GI tract which directly affect symptomology. These identified species secrete a greater number of lipopolysaccharides, a digestive toxin, which is associated with increased inflammatory markers identified in bipolar symptomatology.
This adversely stimulates the central nervous system, specifically the limbic system via a vagal response.
This gut biome imbalance further inhibits the body’s ability to regulate serotonin, GABA, and other neurotransmitters, responsible for appropriate mood regulation.
Using simple treatments like psychobiotics, or probiotics, are resulting in positive gut microbe responses in those who suffer from bipolar.
For those who are prone to repeated hospitalizations due to bipolar mania, relief has been identified from microbiome targeted probiotics. As highlighted in the medical journal, Bipolar Disorder (2018).
Oxidative stress, due to “lipopolysaccharide-induced-inflammation,” adversely affects “glutamate neurotransmission.” Which negatively affects neuroprotective pathways and results in bipolar symptomatology.
Published in Neuroscience and Biobehavioral Reviews, 2011, researches pointed out the positive role N-acetyl cysteine (NAC), an over the counter antioxidant, has on glutamate - the body’s master antioxidant compound.
Progressive research is indicating that non-medication interventions, such as probiotics, antioxidants and many others, are having positive effects on peripheral nervous system inflammatory pathways.
Peripheral inflammation is directly related to the epigenetic expression in bipolar disease, by dysregulating the central nervous system by pro-inflammatory compounds that are far removed from the central nervous system.
Which is now being understood as the collateral damage caused by developmental trauma.
Reflecting that the management of bipolar disorder may include integrative approaches far removed from the current medical model and gene theory approaches.
Psychotherapy Advances – A New Paradigm in Treatment; Part II.
With the growing tide, and large body of research, times are changing within some mental health academic centers.
Which are beginning to emphasize the need for trauma-informed curriculums and educating upcoming providers on the impact that developmental trauma has on psychotherapeutic approaches.
Ella Rosenthal, a 2017 undergraduate student, published her Honors Degree Thesis for a Bachelor in the Science of Psychology, at the University of Portland. Which is titled Developmental Trauma Disorder & Effective Therapeutic Interventions. Where she states:
“Adult clients who have lived through developmental trauma may have subtle treatment-resistant psychological and psychiatric conditions, therefore may need [novel] forms of [psychotherapy] approaches.”
Ms. Rosenthal further suggests that developmental trauma is more often “overlooked by the field” which has created a risk that …
“40% of those with developmental trauma are commonly and incorrectly diagnosed which result in poor treatment response due to interventions that are not trauma-informed, or trauma based”
Further in her thesis, she cites the American Journal of Orthopsychiatry.
Which discussed in 2012, that therapeutic case conceptualization, among adults who suffer childhood victimization, need to be adjusted for the . . .
Reinforcing Rosenthal’s undergraduate’s work is the findings from Ivan Lucero, Licensed Clinical Social Work, at Simmons College, Boston Massachusetts.
Published in 2018, within the Journal of Child & Adolescent Trauma, Lucero stresses the growing evidence supporting that “transgenerational transmission of trauma” is due to maladaptive caregiver actions, developmental trauma events and adverse childhood experiences.
Which have direct “epigenetic consequences on disease pathology throughout life.”
The Journal for Child and Adolescent Trauma (2018), puts forth the need for sharpened acuity among providers who can identify the “molecular scars” involved in “developmentally sensitive, neurobiology-informed approach(es).”
This allows for specific interventions within a neuro-sequential and developmental stage approaches that accurately pinpoint relational insights among those who have experienced developmental trauma.
Adverse Childhood Experiences & HPA-Axis Dysfunction - connects the peripheral inflammatory cascade that “affect brain development and exert long-term influence on psychopathology,”
Neuropsychopharmacology, 2017.
Therapist, most often, are only trained in verbal, insight and cortical approaches that do not address the relational capacities, and burned in stress response, originating within the diencephalon levels of limbic system.
Submitting that suffers of developmental trauma require psychotherapeutic interventions that also target the Hypothalamus-Pituitary-Adrenal Axis Dysfunction.
That is found in trauma-informed modalities and psychoneuroimmunology approaches.
Within the research of Developmental Trauma Disorder, it has been established that traditional cortical, verbal and insight psychotherapy tactics have decreased efficacy due to altered cortical arousal related to childhood trauma experiences.
Giving rise to the importance of trauma screening, trauma informed care and neuroinflammation psychoeducation.
Significance of the New Paradigm.
Dr. Bessel van der Kolk, while junior faculty at The Harvard School of Medicine Trauma Center, pioneered the science in 1989, that thirty years later continues to reinforce that trauma transmission is more so found in the . . .
The last two decades of developmental trauma, and epigenetic, research has brought forth a new division within the trauma-informed-care model referred to as, psychoneuroimmunology.
Psychoneuroimmunology considers a whole-body approach when treating mental health clients.
Specifically, it is the study of interactions between behavior, neural and endocrine function, and immune processes that have peripheral implications on psychopathology and symptomology.
In that, reducing peripheral inflammation has a significant effect on the reduction of symptoms that are far removed from the inflammatory brain response associated with psychopathology.
Indicating the importance of clinical understandings of the bidirectional inflammatory response.
Which is identified as an connected culprit in both treatment resistance and persistent symptoms found in some clients.
Conjointly used, in developmental trauma approaches, is also trauma informed psychotherapy. That carefully identifies the subconscious, ingrained developmental stages, and established adaptations, that are created due to childhood maltreatment and stress.
Where specific, trauma informed care interventions recognize the unique needs of clients who suffer from Developmental Trauma Disorder.
Through this “epigenetically-informed lens” trauma informed psychotherapists are provided the tools that construct a trauma map, allow for effective “bottom-up” and carefully timed “top-down” interventions that are needed for those clients who have been exposed to transgenerational transmission of trauma.
This provides for a precise, effective, up to date, and applicable treatment care model that is truly client focused.
Looking past the Genetic and Genome Theories are the 21st century, neurobiological confirmations signifying the impact of childhood trauma and epigenetics.
Which has strengthened the acceptance of the Developmental Trauma Disorder.
Demonstrating that epigenetics and trauma transmission, not inherited traits, play a substantial role in the risk and development of psychopathology.
Reinforcing that proper developmental assessment and a whole body, trauma-informed approach is the new-paradigm.
Commentary – The New Paradigm
19th Century, French Neurologist, Jean Martin Charcot was the first to be recognized for his work with Trauma Theory and deserves greater recognition.
Long after his first publications in the 1980’s identifying childhood trauma, Psychiatrist Bessel van der kolk, M.D., has became known as the modern-father of developmental trauma.
Over thirty years later, his work still continues today.
Putting forth contemporary research revealing the damaging effects of developmental trauma.
As indicated in this 2019 publication, where he firmly strengthens
“a strong association between exposure to childhood victimization and psychopathology.”
In that, those who meet criteria for Developmental Trauma Disorder are associated with comorbidities that “extend beyond those of PTSD.”
Highlighting, in the most current research, that those who suffer developmental trauma have more severe risk factors, and problematic pathology, than those exposed to shock-trauma associated with a PTSD diagnosis.
It is time to shed light on the fact that most mental health clinics, most graduate level psychology programs, most mental health practice magazines, and sadly most clinicians, have yet to catch up with the enormous amount of peer reviewed science delivered in the past two, even three, decades.
Which looks past the current, allopathic, medical, genetics and symptom based models.
Who reinforce the well taught, yet important, verbal, insight, and cortical focused psychotherapeutic interventions.
It is time look into the Adverse Childhood Experiences and the epigenetic research which connects developmental trauma its effects among those who suffer years and decades after the event(s).
While also recognizing that most therapy clients, as the science points out, has concomitant, bidirectional inflammatory responses that perpetuate chronic symptomatology that can exhibit as treatment, yet treatable, resistance.
Dr. Vincent Felitti, the person who started it all - the father of Kaiser’s Adverse Childhood Experiences (ACEs) research - discovered the link between childhood maltreatment and disease.
As early as 1998 he establish . . .
Some twenty two years later, are the scientific contributions of academic authors, who pointing out in a segment within the book, Contemporary Developmentments and Perspectives in International Health Security,” that:
“contributions of ACEs associated chronic diseases” and the “consequential physiologic and biomolecular changes explained by the Biological Embedding of Childhood Adversity Model.”
Reinforcing the research, published six years earlier, that submits that if childhood victimization is linked to both psychopathology and chronic diseases, then addressing developmental trauma within a trauma-informed care model is indeed . . .
(quoted two years after the publication of the DSM-5)As trauma-informed psychotherapist, who is also credentialed in Psychoneuroimmunology, I have a burning passion to move forward these new paradigms, and novel discussions, within mental health care.
That I, firsthand, have witnessed can disorientate both the conventional and the unaware within the current therapy establishment.
It is time to recognize that the old paradigm is accompanied by static standards within the field of psychotherapy.
Which recognizably impedes not only the trauma survivor from healing, but just as importantly, it further stunts the clinician from meeting their client where they truly are and where they have always been.
In that adaptive, yet subconscious, protective space where the injury has been protected and hidden . . .
. . . yet, precisely where healing must begin.